For the past decade, fentanyl has been the leading cause of drug overdose deaths in the United States. This crisis began quietly around 2014, when illicitly manufactured fentanyl (IMF), much of it sourced from Asia and later trafficked through Mexico, entered the U.S. drug supply.
Today, fentanyl is responsible for an unprecedented wave of fatalities.
Fast fact: By August 2023, fentanyl was killing nearly 80,000 Americans every year (CDC). That means a single synthetic opioid is claiming more lives annually than car accidents or gun violence.
But why is fentanyl so dangerous, and what can people do to stay safe? Let’s break it down.
What Is Fentanyl?
Fentanyl is a synthetic opioid, a man-made drug in the same class as morphine and heroin. In hospitals, it’s prescribed for severe pain, such as post-surgery or late-stage cancer.
This pharmaceutical fentanyl is carefully dosed and administered under medical supervision.
The real danger comes from illegally manufactured fentanyl (IMF). This version is made in clandestine labs, pressed into counterfeit pills, or mixed with heroin, cocaine, or meth. Because it’s so cheap and so potent, drug traffickers use it to stretch their supply.
The problem is, users rarely know they’re taking it and that risk is often fatal.
Overdose Risk: How much Fentanyl is Lethal
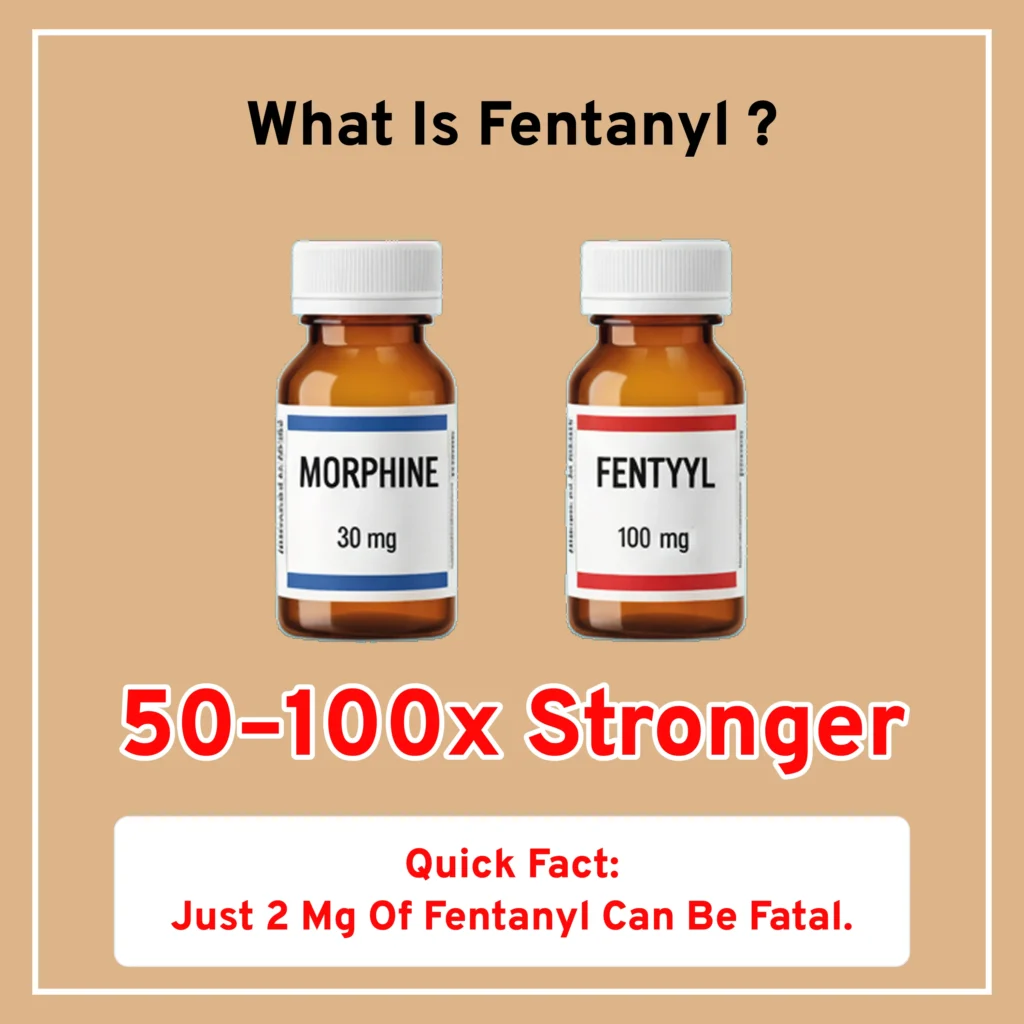
Fentanyl is 50 to 100 times more potent than morphine. It works by binding tightly to opioid receptors in the brain, the same receptors that control pain and regulate breathing. In high doses, fentanyl slows breathing to the point of respiratory depression, the body simply stops getting enough oxygen.
This is why fentanyl overdoses often turn deadly within minutes.
Overdose Symptoms:
Recognizing an overdose quickly can save a life. Common signs include:
- Pinpoint pupils
- Loss of consciousness
- Slow or stopped breathing
- Blue or gray lips and skin
Lethal Dose:
The amount of fentanyl needed to cause death is shockingly small. As little as 2 milligrams, about a few grains of salt can be enough to kill an average adult (DEA).
Hidden in Other Drugs: The Unintentional Risk
One of the greatest dangers of fentanyl is that people often don’t realize they are taking it at all. Unlike prescription fentanyl that is carefully measured in micrograms, illicit fentanyl is usually mixed into street drugs with no quality control.
Dealers frequently cut fentanyl into heroin, cocaine, or methamphetamine to make their supply stronger and cheaper to produce. It’s also commonly pressed into counterfeit pills that are made to look identical to prescription medications such as Xanax, OxyContin, or Percocet. To the user, there is no visible difference, but the risk is astronomical.
The amount of fentanyl in these counterfeit drugs varies wildly. Laboratory testing has found:
- 6 out of 10 fake prescription pills seized on U.S. streets contained a potentially lethal dose of fentanyl.
- A single counterfeit pill can contain anywhere from 0.02 mg to over 5 mg of fentanyl. Remember, just 2 mg is enough to kill an adult.
- In powder form, users might get “hot spots” where fentanyl is unevenly mixed — meaning one line or hit could carry a fatal dose even if previous ones did not.
This unpredictability is what makes unintentional fentanyl use so deadly. Someone who thinks they are taking a Xanax for anxiety, an OxyContin for pain, or even just “a bump” of cocaine at a party could unknowingly ingest enough fentanyl to stop their breathing within minutes.
NIDA reports that many overdose victims never realized fentanyl was in their system until toxicology confirmed it. This hidden danger explains why overdose deaths have risen so sharply since 2014 — people aren’t “choosing fentanyl” in many cases; they are unknowingly exposed to it.
The reality is simple: any pill or powder bought outside a pharmacy carries the risk of being contaminated with fentanyl. That’s why test strips, naloxone, and immediate emergency response are so critical in preventing deaths.
Addiction Potential: What it does to You
Fentanyl addiction is not just dangerous because of the risk of overdose, it’s also one of the most addictive drugs ever made. Like other opioids, it works by binding to the brain’s opioid receptors, releasing a powerful surge of dopamine, the “feel good” chemical that regulates reward and motivation. This creates intense euphoria but also rewires the brain to crave fentanyl again and again.
Because fentanyl is 50–100 times stronger than morphine, this rewiring happens much faster than with other opioids. Even a short period of use can lead to physical dependence, meaning the brain and body cannot function normally without the drug. Once dependence sets in, stopping fentanyl brings on severe withdrawal symptoms, which often trap people in a cycle of continued use.
How Fentanyl Affects the Body and Bran:
Long-term fentanyl use doesn’t just change behavior, it damages nearly every organ system:
- Brain: Alters reward pathways, making everyday pleasures (food, relationships, hobbies) feel meaningless compared to the drug. It reduces impulse control, fuels compulsive use, and increases the risk of anxiety, depression, and cognitive decline.
- Lungs: Fentanyl suppresses breathing. Over time, chronic oxygen deprivation (hypoxia) and weakened lung function raise the risk of pneumonia, infections, and even permanent brain damage from lack of oxygen.
- Stomach and Digestive System: Like other opioids, fentanyl slows digestion, leading to severe constipation, nausea, abdominal bloating, and chronic stomach pain. Some people develop “opioid bowel syndrome,” a painful and debilitating condition.
- Skin: Regular use can cause itching, rashes, excessive sweating, and, in cases of injection drug use, painful abscesses or lesions due to contaminated needles or toxic cutting agents.
- Eyes: Pinpoint pupils are one of the telltale signs of opioid use. Over time, fentanyl can cause blurred vision, sensitivity to light, and vision disturbances.
This is why fentanyl addiction is often described as a “hijacking of the brain”, it changes how people think, feel, and behave at a biological level. Breaking free almost always requires professional treatment, medical detox, and ongoing support, since the drug’s hold is both physical and psychological.
Withdrawal: Painful and Dangerous
When someone who is dependent on fentanyl stops using, withdrawal symptoms can appear within hours. They are extremely uncomfortable and often push people back into use.
Common withdrawal symptoms include:
- muscle and bone pain
- vomiting
- diarrhea
- cold flashes
- insomnia
- uncontrollable cravings.
While withdrawal itself is usually not fatal, it can be so severe that medical detox, Fentanyl treatment or medication-assisted treatment (MAT), such as buprenorphine or methadone, is recommended.
Fentanyl doesn’t give second chances but recovery does. If you or a loved one is struggling with fentanyl use, professional help can save a life. Don’t wait until it’s too late.
Staying Safe: Harm Reduction Strategies for Fentanyl
Even for people who aren’t ready to quit fentanyl or other substances, there are practical steps offered at Rehab Centers that can reduce the risk of overdose and death. These harm reduction tools don’t encourage drug use, they save lives by giving people a second chance at recovery.
Naloxone (Narcan): The Overdose Reversal Medication
Naloxone, often sold under the brand name Narcan, is a fast-acting medication that can reverse the effects of an opioid overdose by quickly binding to opioid receptors in the brain. It works within minutes, restoring normal breathing and consciousness.
With fentanyl, however, overdoses are often more severe than with heroin or prescription painkillers. Because fentanyl is so potent, multiple doses of naloxone may be needed to revive someone. For this reason, it’s best to have more than one dose on hand if you live with, or love, someone at risk of fentanyl use.
Today, naloxone is much more accessible:
- It is available without a prescription in most states, often at pharmacies.
- Community organizations and harm reduction programs sometimes distribute it for free.
- Groups like NEXT Distro even mail free naloxone kits in certain areas.
Having naloxone nearby can be the difference between life and death. Experts recommend that anyone who uses opioids, or lives in a community affected by fentanyl, carry it just in case.
Fentanyl Test Strips: A Simple Line of Defense
Another important harm reduction tool is the fentanyl test strip. These small strips can be dipped into a drug sample dissolved in water to check if fentanyl is present. If the strip turns positive, it means the drug supply is contaminated.
Why this matters:
- Many people who overdose on fentanyl never intended to take it, it was hidden in counterfeit pills, heroin, meth, or cocaine.
- Using test strips can help people avoid a deadly mistake.
However, test strips are not perfect. They may not detect every fentanyl analog (chemical variations like carfentanil), and results depend on how well the drug was mixed. Still, research shows that people often change their behavior after a positive test, for example, using less, using with others nearby, or deciding not to use at all.
Call 911 First: The Most Important Step
If you ever suspect someone is overdosing on fentanyl, call 911 immediately before doing anything else. An overdose is a medical emergency, and seconds matter.
Signs of a fentanyl overdose include:
- Slow or stopped breathing
- Pinpoint pupils
- Blue or gray skin, lips, or nails
- Unconsciousness or inability to wake up
Once you’ve called for help, administer naloxone if available, and begin rescue breathing or CPR if you are trained. Emergency responders can provide oxygen, advanced airway support, and additional naloxone doses if needed.
Remember: Don’t wait to see if someone “snaps out of it.” Fentanyl acts quickly, and the window to save a life is often very short.
Fentanyl and the Opioid Crisis
Fentanyl is not America’s first opioid crisis, but it is by far the deadliest and fastest moving. The U.S. has battled waves of opioid misuse for decades, from the rise of prescription painkillers in the 1990s to the surge in heroin use in the 2000s. But fentanyl has changed the landscape completely.
Unlike heroin or morphine, which require larger amounts to produce a high, fentanyl’s extraordinary strength makes it uniquely risky. Just two milligrams, about the size of a few grains of salt, can be lethal. This razor-thin margin between a “dose” and an overdose explains why deaths have skyrocketed.
How Fentanyl Took Over the Illegal Drug Market
The Centers for Disease Control and Prevention (CDC) reports that synthetic opioids like fentanyl are now the leading cause of overdose deaths in the U.S., killing nearly 80,000 people in 2023 alone. Most of these deaths involve illicitly manufactured fentanyl (IMF), not prescription fentanyl from hospitals.
Here’s how the illegal market drives the crisis:
- Sourcing and Trafficking: Much of the raw fentanyl and its chemical precursors are produced overseas, particularly in China and Mexico. Mexican cartels often manufacture fentanyl in clandestine labs using precursor chemicals shipped from Asia, then smuggle it across the U.S. border.
- Low Cost, High Profit: Fentanyl is cheap to produce compared to heroin. Just a few kilograms can yield millions of doses, making it extremely profitable for dealers.
- Cut Into Other Drugs: Dealers mix fentanyl into heroin, cocaine, and meth to boost potency, or press it into counterfeit pills designed to look like real prescriptions (like Xanax or OxyContin). Users often have no idea they are taking fentanyl until it’s too late.
- Unpredictable Purity: Unlike regulated pharmaceuticals, street fentanyl has no quality control. A single batch may contain wildly different concentrations, leading to “hot spots” of extremely potent powder — one line, pill, or injection can kill instantly.
Addiction doesn’t define your future, recovery does. Whether it’s fentanyl, opioids, or any other substance, the right support can help you take back control of your life.
How long does fentanyl stay in your system?
Fentanyl leaves the body quickly but depends on use: up to 12 hours in blood, 1–3 days in urine, and 90 days in hair. Even after it’s gone, cravings and withdrawal can last longer.
What happens at the end of fentanyl rehab?
Rehab ends with detox, therapy, and relapse-prevention tools, but recovery continues. Most people move into aftercare — like counseling, sober living, or support groups — to stay on track.
What is fentanyl treatment?
Treatment combines medications (like buprenorphine or methadone) to reduce cravings with therapy and support to address the root causes of addiction. The best plans are personalized.
Does fentanyl make you sleepy?
Yes. Fentanyl often causes drowsiness and sedation. While common, extreme sleepiness with slow breathing can signal an overdose and requires immediate medical help.
What drugs are used for fentanyl addiction recovery?
Common medications include buprenorphine, methadone, and naltrexone. They reduce cravings, ease withdrawal, or block fentanyl’s effects, making recovery more manageable.


