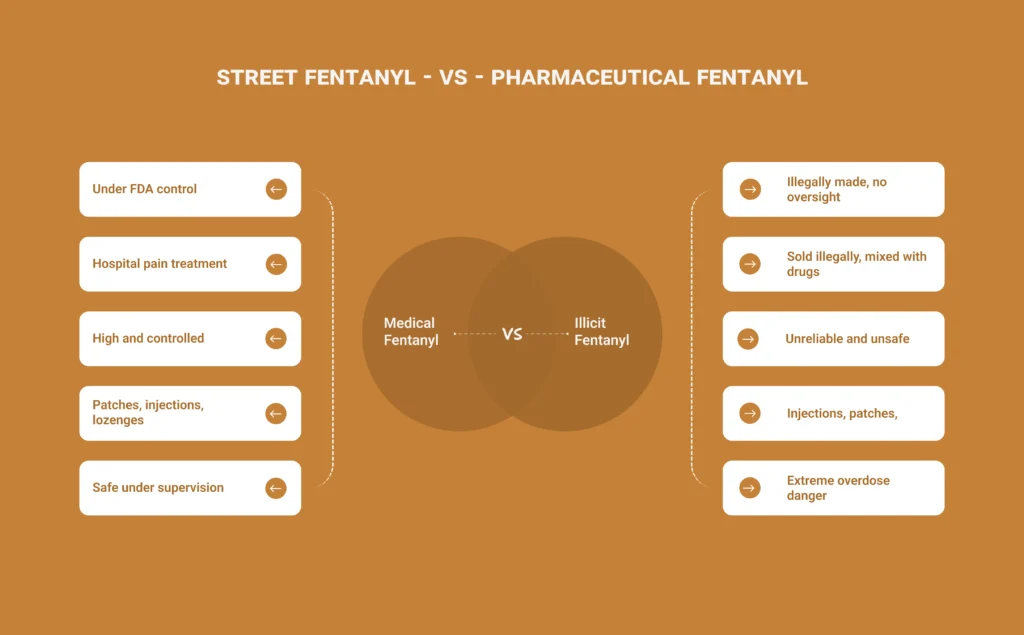
Fentanyl is one of the most talked-about substances in the world today and for good reason. It’s a life-saving medication in hospitals but also one of the deadliest drugs on the streets. The difference between street fentanyl vs pharmaceutical fentanyl can literally mean the difference between treatment and tragedy.
What is pharmaceutical Fentanyl and How Is It Used in Hospitals?
Pharmaceutical fentanyl, often referred to as medical fentanyl, is a powerful synthetic opioid originally developed in 1959 by Dr. Paul Janssen. It was designed to treat severe and chronic pain that couldn’t be managed by other opioids like morphine or oxycodone.
In medical practice, fentanyl is 50 to 100 times stronger than morphine, meaning it’s effective in extremely small doses. Because of this potency, it plays a crucial role in hospital pain management, particularly in post-surgical recovery, emergency care, cancer treatment, and intensive care units (ICUs).
How It Works in Medical Settings
When used in hospitals, pharmaceutical fentanyl binds to the brain’s mu-opioid receptors, the same receptors responsible for controlling pain and emotions. By activating these receptors, it blocks pain signals, providing rapid relief for patients in critical pain.
Medical fentanyl is available in several regulated forms, including:
- Intravenous (IV) injections – Commonly used in operating rooms or emergency situations for immediate pain control or anesthesia.
- Transdermal patches (Duragesic) – Designed to release fentanyl slowly through the skin over several days for chronic pain management.
- Lozenges or lollipops (Actiq) – Used for “breakthrough pain” in cancer patients already on opioid therapy.
- Nasal sprays or buccal tablets – Occasionally prescribed for patients with severe, recurring pain episodes.
Every dose of hospital-grade fentanyl is meticulously calculated, prescribed, and administered by healthcare professionals. Patients are closely monitored for side effects like slowed breathing, drowsiness, or nausea, which can occur even with medical use.
Because of its strength, medical fentanyl is never given casually. It’s reserved for cases where the benefit outweighs the risk, such as trauma, advanced-stage cancer, or major surgery recovery.
So yes, hospitals do give fentanyl, but it’s done with strict supervision, sterile manufacturing standards, and precise dosing protocols that make it safe and effective when used properl
What Is Street Fentanyl?
Street fentanyl, also known as illicit fentanyl or fentanyl-laced drugs, is a non-medical version of the drug made illegally in unregulated laboratories, often overseas or in hidden local setups. Unlike pharmaceutical fentanyl, which is produced under FDA-regulated conditions, street fentanyl is created with no quality control, no accurate dosage, and no safety testing.
How Street Fentanyl Is Made and Sold
Illicit fentanyl is typically synthesized using cheap precursor chemicals and then sold in different forms, most commonly as a powder, counterfeit pill, or liquid.
Dealers and traffickers often mix it with other substances such as:
- Heroin (to increase potency and addictiveness)
- Cocaine or methamphetamine (to stretch supply and boost profits)
- Pressed pills that mimic real medications like OxyContin, Xanax, or Percocet
Because it’s so potent, even 2 milligrams of fentanyl, an amount smaller than a few grains of salt, can cause a fatal overdose. Users rarely realize how much they’re taking because street fentanyl has no distinct smell or taste, and its concentration varies wildly from batch to batch.
Why Street Fentanyl Is So Dangerous
- Unpredictable potency: There’s no way to tell how strong each dose is.
- Lack of regulation: It’s produced in unsanitary, unsafe environments without medical oversight.
- Hidden presence: It’s often mixed into non-opioid drugs without users’ knowledge.
- Rapid onset: Fentanyl acts fast, sometimes within seconds, giving little time for emergency help.
This unpredictability makes illicit fentanyl the leading cause of opioid-related overdoses in the U.S. and Canada today. According to the CDC, the vast majority of recent overdose deaths involve synthetic opioids like fentanyl, not prescription versions.
In short, while medical fentanyl saves lives when used responsibly in hospitals, street fentanyl destroys lives because it’s unregulated, contaminated, and lethal even in trace amounts.
What Does Street Fentanyl Look Like?
There’s no single way to identify street fentanyl, which is part of what makes it so deadly. It can appear as:
- White or off-white powder
- Pills that mimic legitimate prescription opioids
- A sticky residue or liquid form
- Pressed tablets resembling OxyContin, Percocet, or Xanax
Because it’s odorless and tasteless, there’s no reliable way to tell street fentanyl apart from other substances without using fentanyl test strips, which can detect its presence in powders and pills.
When Did Fentanyl Hit the Streets?
History of fentanyl tells us, while fentanyl was first approved for medical use in the 1960s, illicit fentanyl began appearing in the 1990s, with a major surge in 2013–2014 when black-market labs started mass-producing synthetic opioids.
Since then, street fentanyl has been linked to a dramatic rise in overdose deaths across North America and beyond. According to the CDC, synthetic opioids, primarily illicit fentanyl, are now the leading cause of opioid-related deaths.
Is Medical Fentanyl Different from Street Fentanyl?
Yes and the difference is critical.
Medical fentanyl is:
- Pure, controlled, and regulated by health authorities
- Administered by trained professionals
- Meant to relieve suffering safely
Street fentanyl, on the other hand, is:
- Illegally made and sold
- Often contaminated or misrepresented
- Responsible for the majority of current opioid overdoses
In short, street fentanyl is not the same as hospital fentanyl and using them interchangeably can be deadly.
The Impact on Public Health
The public health impact of street fentanyl has been catastrophic. According to the CDC, synthetic opioids, primarily illicit fentanyl, are now responsible for over 70% of all opioid-related overdose deaths in the United States. Between 2013 and 2023, the death rate involving fentanyl increased more than 20-fold.
Key factors driving this crisis include:
- Unpredictable potency: Street fentanyl varies wildly in concentration, making it easy to overdose even with minimal use and immediate fentanyl addiction treatment.
- Widespread contamination: Illicit fentanyl is often mixed with other substances, turning recreational drugs into deadly traps.
- Rapid onset and respiratory failure: Fentanyl’s effects hit within seconds, leaving users little time to respond to overdose symptoms.
- Limited awareness: Many users are unaware that the drugs they purchase contain fentanyl at all.
The National Institutes of Health (NIH) and Substance Abuse and Mental Health Services Administration (SAMHSA) have classified fentanyl-related deaths as a national public health emergency, prompting expanded harm reduction programs, wider naloxone (Narcan) distribution, and community-based prevention efforts.
Despite these initiatives, fentanyl continues to claim thousands of lives annually, with its presence spreading beyond North America to parts of Europe, South Asia, and Australia.
A Global Wake-Up Call
The spread of street fentanyl has transformed what was once a domestic addiction crisis into a global public health emergency. Governments and healthcare providers worldwide are now focusing on:
- Increasing public awareness about illicit fentanyl’s dangers
- Expanding access to addiction treatment and recovery programs
- Promoting fentanyl test strips and overdose reversal medications
- Strengthening law enforcement efforts to curb illegal manufacturing
The story of fentanyl is no longer just about addiction, it’s about how one synthetic drug reshaped global health policy, law enforcement, and our understanding of drug safety.
Protecting Yourself and Others
Education and awareness are the first steps in reducing harm.
Here’s what experts recommend:
- Never test drugs by taste or smell. Fentanyl is odorless and tasteless.
- Use fentanyl test strips before consuming any street-bought substance and visit a Drug Rehab Center for further help.
- Keep naloxone accessible, it can save a life during an overdose.
- Call emergency services immediately in case of suspected overdose.
Is medical fentanyl different from street fentanyl?
Yes. Medical fentanyl (pharmaceutical fentanyl) is a regulated pain medication used in hospitals under strict supervision. Street fentanyl, or illicit fentanyl, is made illegally with no quality control and is often mixed with other drugs, making it unpredictable and deadly.
Is fentanyl used in hospitals?
Yes, fentanyl is used in hospitals to treat severe pain during surgery, trauma, or cancer care. It’s given in precise doses through injections, patches, or lozenges and monitored closely by medical professionals.
What does street fentanyl look like?
Street fentanyl can appear as a white powder, liquid, or fake pills that resemble OxyContin, Xanax, or Percocet. It’s usually odorless and tasteless, which makes it impossible to identify without fentanyl test strips.
How long has fentanyl been on the streets?
Illicit fentanyl appeared in the 1990s and surged around 2013–2014 when black-market labs began mass-producing it. Today, it’s the main cause of opioid-related overdoses in North America, according to the CDC.
Is street fentanyl the same as hospital fentanyl?
No. Hospital fentanyl is pure, controlled, and safely administered by doctors. Street fentanyl is illegal, contaminated, and often mixed with other drugs, making it far more dangerous.
What makes illicit fentanyl so dangerous?
Illicit fentanyl is deadly because of its unpredictable potency and contamination. Even 2 milligrams, about a few grains of salt—can be fatal. It’s fast-acting, often hidden in other drugs, and has no consistent dosage or regulation.


