When people hear the words morphine vs fentanyl, they often think of two of the most powerful pain-relieving drugs in modern medicine. Both are opioids, prescribed to ease moderate to severe pain, especially in situations such as surgery recovery, cancer treatment, or hospice care. But while they may seem similar, fentanyl vs morphine is a comparison that reveals important differences in strength, safety, and medical use.
Morphine, derived from the opium poppy, has been used for centuries as the “gold standard” for pain control. Fentanyl, on the other hand, is a fully synthetic opioid created in laboratories and is significantly stronger, up to 100 times more potent than morphine. Because of this, fentanyl requires careful prescribing and monitoring, but it also offers unique benefits, particularly in hospice and palliative care where fentanyl patches are often used instead of morphine drops.
Fentanyl is more potent than morphine, only a healthcare professional can determine whether fentanyl or morphine is a better option for a person’s medical needs, pain levels, and lifestyle.
What Is Morphine?
Morphine is a naturally occurring opiate, extracted from the sap of the opium poppy. It has been one of the most widely used painkillers in history and is considered the reference point against which the potency of all other opioids is measured. When doctors talk about opioid conversions, they often calculate them in “morphine milligram equivalents” (MME).
Clinically, morphine is prescribed to treat moderate to severe pain, particularly after surgery, during cancer treatment, or for long-term pain management in palliative care. Because it is slower-acting compared to fentanyl, morphine provides a longer duration of pain relief, which makes it reliable for steady pain management.
What Is Fentanyl?
Fentanyl is an addictive, synthetic opioid, first developed in the 1960s. Unlike morphine, which is plant-derived, fentanyl is fully man-made and designed to act quickly and powerfully. Fentanyl is about 50 to 100 times more potent than morphine.
Because of this extreme strength, fentanyl is not usually a first-choice opioid. Instead, it is prescribed in cases of severe pain, often for patients who are already tolerant to other opioids. It is commonly used during surgical procedures, in intensive care, and in hospice or cancer care where traditional painkillers may no longer work effectively.
Unfortunately, illicit fentanyl, produced outside of medical use has become one of the main drivers of the opioid overdose crisis worldwide, making it both a vital medicine and a dangerous substance when misused.
What Forms Do They Come In?
Both morphine and fentanyl are available in different forms depending on the patient’s needs and medical setting.
Morphine can be taken as oral tablets, liquid solutions, or given as injections and intravenous infusions in hospital environments.
Fentanyl, due to its potency, comes in more specialized forms. It is available as injections, nasal sprays, lozenges (sometimes called “lollipops”), and most importantly, fentanyl patches, which deliver a slow and steady dose through the skin over 72 hours. This makes fentanyl especially useful in hospice care, where consistent pain relief is critical.
What Is the Standard Dosage?
Morphine doses vary depending on the severity of pain, but they are usually prescribed in milligrams. Because morphine serves as the baseline for opioid equivalence, it is often used in dosage conversion tables.
Fentanyl dosage, by contrast, is measured in micrograms because of its strength. A typical fentanyl patch may release 12 to 100 micrograms per hour and lasts up to three days. Injectable fentanyl is often given in doses of 50 to 100 micrograms, particularly in surgical anesthesia.
This highlights the vast potency of fentanyl vs morphine, a microgram of fentanyl can equal milligrams of morphine in effect.
How Strong Is Fentanyl Compared to Morphine?
When comparing morphine versus fentanyl, the question most people ask is: is fentanyl better than morphine, or is morphine stronger than fentanyl? The answer depends on context.
Fentanyl is significantly stronger than morphine. In fact, a 25 microgram per hour fentanyl patch provides pain relief similar to 60 to 90 milligrams of oral morphine per day. This means fentanyl is not “better” in all cases, it is simply more potent, which makes it useful for patients who no longer respond to morphine.
However, its potency also makes it more dangerous, as even small mistakes in dosage can result in overdose. For this reason, fentanyl is usually prescribed only to patients with a demonstrated opioid tolerance.
Side Effects and Withdrawal Symptoms of Fentanyl and Morphine usage
Both morphine and fentanyl can cause side effects, many of which are common to all opioids.
Short-term effects of both drugs include:
- drowsiness
- constipation
- fatigue
- paranoia
- nausea and upset stomach
- slowed breathing
In higher doses, they can cause confusion or dangerous respiratory depression.
Long-term use of either drug may lead to:
- tolerance, meaning patients need higher doses over time
- dependence, where the body adapts to the drug and withdrawal occurs if it is stopped suddenly.
- Some patients also develop opioid-induced hyperalgesia, a condition where long-term opioid use actually increases sensitivity to pain.
Withdrawal Symptoms
Stopping opioids like morphine or fentanyl suddenly can trigger uncomfortable withdrawal symptoms. These include:
- anxiety
- sweating
- restlessness
- nausea
- abdominal cramps
- insomnia
- increased blood pressure
While opioid withdrawal is rarely life-threatening, it can be extremely distressing and often requires medical supervision.
Because fentanyl is more potent, withdrawal from fentanyl can feel more severe than withdrawal from morphine.
Take the first step towards safer pain management
If you or your loved one is struggling with opioid use or searching for safer pain management options, help is available.
Overdose Risks and symptoms
Both morphine and fentanyl carry the risk of overdose, but fentanyl is particularly dangerous because of its extreme potency. An overdose can lead to slowed or stopped breathing, extreme drowsiness, unresponsiveness, and in many cases, life threatening complications.
One of the most recognizable signs is pinpoint pupils, often described as “tiny pupils,” along with bluish lips or fingertips due to lack of oxygen. If left untreated, overdose can quickly become fatal.
The emergency treatment for an opioid overdose is naloxone (Narcan), a medication that rapidly reverses the effects of opioids by restoring normal breathing.
However, because fentanyl is so strong, multiple doses of naloxone may be required before a patient stabilizes. Immediate medical attention is critical in these situations, as every minute can make the difference between life and death.
While reversing an overdose is the first step, long-term safety requires addressing the underlying addiction. After emergency care, many patients benefit from entering a structured Fentanyl addiction treatment program, which may include inpatient or outpatient rehab, medication-assisted treatment (such as methadone, buprenorphine, or naltrexone), and behavioral therapies like cognitive behavioral therapy (CBT).
Addiction recovery also involves family support, relapse prevention planning, and ongoing counseling to reduce the likelihood of another overdose and help patients rebuild their lives.
Fentanyl Hospice Patches vs Morphine Drops
In hospice and palliative care, fentanyl patch hospice treatments are often used as an alternative to morphine drops. This is especially helpful for patients who cannot swallow medications or who require round-the-clock pain relief.
Guidelines recommend that fentanyl patches be applied to clean, dry skin every 72 hours. Patients and caregivers are advised to avoid external heat sources like heating pads or hot baths, as heat can increase drug absorption and cause accidental overdose. When switching from morphine to fentanyl patches, doctors carefully calculate the equivalent dosage to avoid under- or over-treatment.
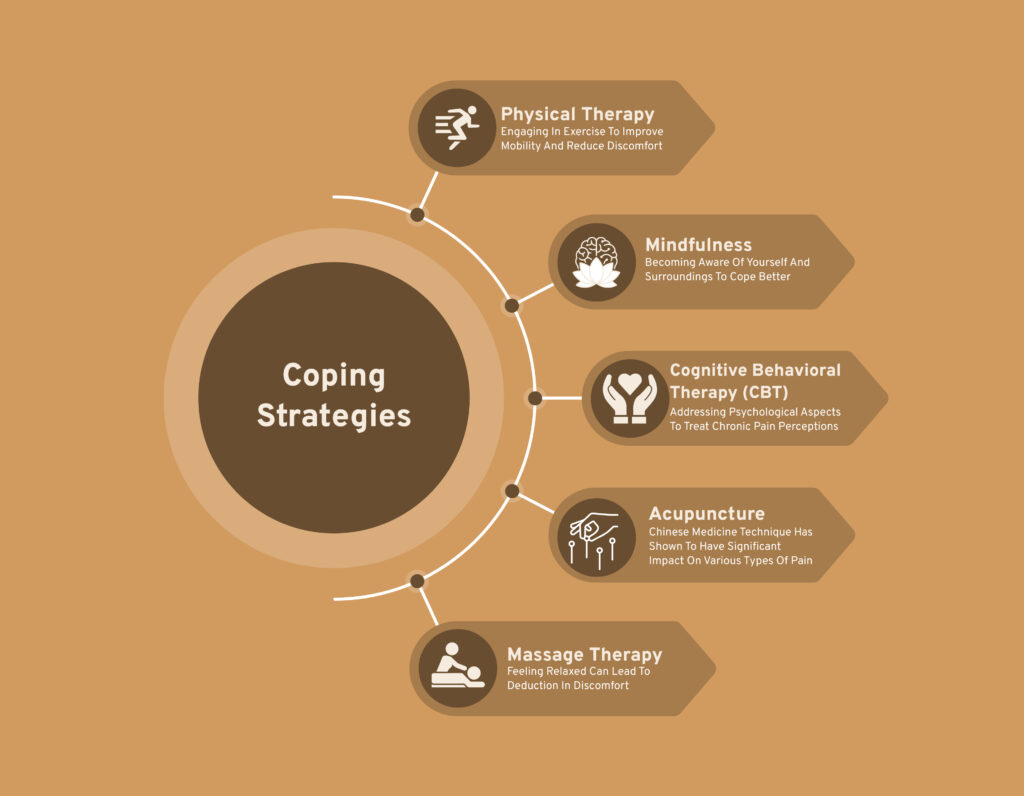
Coping Strategies Beyond Opioids
While morphine and fentanyl are invaluable for severe pain, doctors also encourage non-opioid strategies to minimize risks.
Alternatives may include acetaminophen, NSAIDs, antidepressants, and anticonvulsants for nerve pain.
Non-medication approaches like:
- Physical Therapy – engaging in exercise to improve mobility and reduce discomfort
- Mindfulness – becoming aware of yourself and surroundings to cope better
- Cognitive Behavioral therapy (CBT) – addressing psychological aspects to treat chronic pain perceptions
- Acupuncture – Chinese medicine technique has shown to have significant impact on various types of pain
- Massage therapy – feeling relaxed can lead to deduction in discomfort
can also be integrated into pain management plans.By combining medical alternatives, therapeutic approaches, and where necessary, professional rehab center in Florida, patients can often reduce their reliance on opioids while still maintaining quality of life and regaining a greater sense of control over their health.
Legal Landscape Surrounding Opioids
Both morphine and fentanyl are Schedule II controlled substances under U.S. federal law. This means they have legitimate medical uses but also a high potential for abuse and dependence. Strict regulations govern their prescription, dispensing, and monitoring.
Unfortunately, illicit fentanyl, often mixed with heroin or counterfeit pills, is a leading driver of the opioid crisis, contributing to thousands of overdose deaths each year. According to the DEA fentanyl fact sheet, understanding the difference between medical and illegal fentanyl is critical for patients and families.
Your Recovery starts here!
Why change from morphine to fentanyl?
Doctors may switch patients from morphine to fentanyl if morphine is no longer effective or causes difficult side effects. Fentanyl is often preferred in kidney failure because it does not build up in the body like morphine. It can also be better tolerated in patients who experience nausea or discomfort with morphine, making it a safer and more effective option in certain cases.
What painkiller is stronger than morphine?
Fentanyl is significantly stronger than morphine. In fact, when comparing fentanyl vs. morphine, fentanyl’s potency is one of the reasons it is prescribed for patients who need rapid or more intense pain relief. However, its strength also comes with higher risks of dependence, overdose, and severe side effects, which is why it is only used under strict medical supervision.
Is fentanyl better than morphine for kidney failure?
Yes, fentanyl is often considered safer than morphine for patients with kidney failure. Morphine is metabolized by the kidneys, which can lead to toxic buildup in patients with impaired kidney function. Fentanyl, on the other hand, is primarily processed by the liver and does not accumulate in the kidneys in the same way. For this reason, many doctors prefer prescribing fentanyl patches or injections for pain management in kidney failure patients.
Does fentanyl cause less nausea than morphine?
In many cases, yes. While both morphine and fentanyl can cause nausea, studies and patient experiences suggest that fentanyl is often better tolerated in this regard. Morphine is more likely to trigger gastrointestinal side effects such as nausea, vomiting, and constipation. That said, everyone responds differently, and side effects should always be monitored closely by a healthcare provider.
Which is higher, morphine or fentanyl?
When people ask “which is higher,” they usually mean which drug is stronger in terms of potency. The answer is fentanyl. Fentanyl is much more potent than morphine, meaning that a much smaller dose of fentanyl is required to achieve the same pain-relieving effect as a larger dose of morphine. This difference highlights why fentanyl must be handled with extreme caution, as even tiny miscalculations can lead to overdose.


